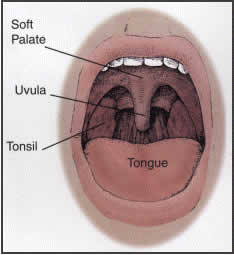
 Snoring is a very common problem, caused by obstruction and vibration of the tissues in the mouth and throat. The cause of snoring can be an elongated soft palate and uvula, large tonsils, a large or floppy tongue, obstructed nasal airways, or collapse of tissues lower in the throat. While simple snoring is an annoying and socially disruptive problem, it can be a sign of obstructive sleep apnea (OSA), a significant medical problem that can lead to daytime sleepiness, morning headaches, interrupted sleep, and even significant heart and lung disease. Patients with OSA may have a higher risk of premature death, especially if they are under 40 years old, have significant heart or lung disease, or are more than 100 pounds overweight. The initial steps in diagnosis are an exam by a head and neck surgeon, as well as an overnight sleep study (polysomnogram) in a sleep laboratory. These tests will help locate the source of obstruction and indicate the severity of the apnea. Click here to take a survey to help determine if you may have sleep apnea.
Snoring is a very common problem, caused by obstruction and vibration of the tissues in the mouth and throat. The cause of snoring can be an elongated soft palate and uvula, large tonsils, a large or floppy tongue, obstructed nasal airways, or collapse of tissues lower in the throat. While simple snoring is an annoying and socially disruptive problem, it can be a sign of obstructive sleep apnea (OSA), a significant medical problem that can lead to daytime sleepiness, morning headaches, interrupted sleep, and even significant heart and lung disease. Patients with OSA may have a higher risk of premature death, especially if they are under 40 years old, have significant heart or lung disease, or are more than 100 pounds overweight. The initial steps in diagnosis are an exam by a head and neck surgeon, as well as an overnight sleep study (polysomnogram) in a sleep laboratory. These tests will help locate the source of obstruction and indicate the severity of the apnea. Click here to take a survey to help determine if you may have sleep apnea.Treatment options
When first line precautions like weight loss, not sleeping on your back, and avoidance of sedatives and alcohol at nighttime fail, there are several options to treat sleep apnea.
Sleep Position: Sleeping on the side can avoid the collapse of the tongue that occurs when sleeping on your back. A sock containing a tennis ball pinned to the back of a t-shirt can help with this.
Continuous Positive Airway Pressure or “CPAP“: By wearing a mask connected to a machine that blows air into the nose and/or mouth, OSA can be effectively treated 99% of the time. It is a safe, painless, and effective treatment. However, many people do not tolerate or like wearing a mask while sleeping, and long-term use rates remain poor.
Dental appliances: By wearing a mouthpiece at night, usually fit by a dentist or orthodontist, the tongue and mouth tissues are held open. This is a safe but less effective option, with success rates ranging between 50-60%. Some people have significant problems with jaw joint pain due to appliance use.
Surgery: There are several different procedures that are commonly done for OSA and snoring.
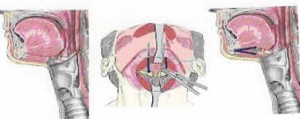
Uvulopalatalpharyngoplasty or UPPP: This procedure targets obstruction of the soft palate by trimming of the palate and uvula, of
ten in conjunction with removal of the tonsils. The palate is then sutured to create an open airway.
Tongue suspension: When tongue collapse is a problem, placement of a small screw in the jaw connected to a permanent stitch through the back of the tongue can help hold the tongue forward and the airway open.
Hyoid Suspension: When collapse lower in the throat is causing apnea, this procedure is done to raise the hyoid bone (located above the “Adam’s apple”) and keep the throat open. This can be done with tying special stitches and securing them to a small screw on the mandible.
Laser Assisted Uvuloplasty or LAUP: A procedure where a laser is used to trim the uvula and palate, usually reserved for snoring or mild apnea only.
Radiofrequency Ablation: An office procedure using needles inserted into the palate, nasal turbinates, or base of tongue. By running radiofrequency energy through the needles, these tissues shrink by heating and scarring over time. It is at this time reserved for nasal congestion, snoring, and mild apnea only. See http://www.somnus.com/MDframePC.html for more information.
Lingual Tonsillectomy: Removal of the tonsils in back of the tongue. These often enlarge after the regular tonsils have been removed.
Injection Snoroplasty: An office procedure for snoring where medication is injected into the soft part of the roof of the mouth under topical anesthetic. This medication causes tightening of the lining tissue making it vibrate less thus controlling snoring. Most patients resume normal activity the following day and have minimal pain.
Uvulectomy: An office procedure done for snoring under local anesthesia. This is most helpful in patients with a long thin uvula but others benefit as well. The uvula interlocks with the voice box in infants allowing nasal breathing while feeding at the same time. These structures grow apart with age and thus the uvula has no real function in adults or even children. There is a mild to moderate amount of pain for several days following the procedure.
Nasal surgery: While nasal blockage can be a factor in snoring and apnea, it rarely is the sole cause. Straightening the septum (Septoplasty) and reducing the size of the nasal turbinates can open the nose and improve breathing.
Surgical therapy can be very effective in certain cases of sleep apnea when there is a clear site of upper airway obstruction. Snoring can be eliminated or significantly improved in 80-85% of patients. Apnea can be eliminated or significantly improved in up to 75% patients; however, long-term results (5 years or longer) reveal significant improvement in 50-55% of patients. The obvious benefit of surgical therapy is a reasonable chance for improved sleep without the need for any machines or appliances.
Surgical Instructions
Preoperative Instructions: Once your doctor has determined that surgical treatment for sleep apnea is indicated, our staff will arrange the surgical date. You may not have anything to eat or drink after midnight prior to your surgery or your procedure may be cancelled. Plan on at least an overnight stay in the hospital for UPPP and/or tongue suspension.
Postoperative Instructions: The majority of patients can be safely discharged to home the day after surgery for OSA. Your surgeon will give you prescriptions for liquid pain medicine, antibiotics, and possibly steroids. The major difficulty after surgery is pain-throat pain, difficulty swallowing, and pain radiating to the ears is very common. This pain can be very severe, but with regular doses of pain medication and plenty of fluids, it can be controlled. The pain usually lasts at least 10-14 days, but occasionally will last longer.
It is crucial to drink plenty of fluids after surgery. Water, Gatorade, Popsicles, and clear juices are the best. Avoid drinks with caffeine or alcohol, as they will dehydrate you. While most people begin taking soft foods within 24-48 hours after surgery, most find they lose a few pounds before being able to resume a normal diet by about two weeks after surgery.
Bleeding is a rare complication after surgery. Occasionally, when healing tissue in the mouth or palate sloughs off, bleeding from the incisions can occur. The majority of the time, this is easily controlled in the office or, if after hours, in the emergency room.
If the palate and uvula are trimmed, initially you may notice a nasal quality to your voice, or have liquids accidentally reflux into your nose while swallowing. This is a problem that very rarely is a long-term problem and improves as the palate heals. In the rare patient where this is persistent, treatments ranging from speech exercises to corrective surgery are available.
If the palate and uvula are trimmed, initially you may notice a nasal quality to your voice, or have liquids accidentally reflux into your nose while swallowing. This is a problem that very rarely is a long-term problem and improves as the palate heals. In the rare patient where this is persistent, treatments ranging from speech exercises to corrective surgery are available.
If tongue suspension is performed, expect some amount of swelling under the tongue that will resolve over one week. Over correction of tongue collapse can cause swallowing problems. Cutting the suture in the office can easily reverse this.
Depending on the procedure, plan on 2 weeks for recovery. You likely will be seen 2-4 weeks in the office after the procedure for follow up. Many surgeons will also repeat your sleep study 3 to 6 months after surgery to evaluate results.